Should I Get Off My Antidepressants? Understanding the Risks and What Science Says
When people begin to feel better after a period of depression, a common question arises: Should I stop taking my antidepressants? It’s a decision many patients bring up during appointments with their psychiatrist. The answer is rarely simple, and it depends on your history, current stability, and risk of relapse.
As a Manhattan psychiatrist who treats adults, adolescents, and members of the LGBT community in NYC, I have this conversation often. This article will walk through the evidence, highlight relapse risks, and share practical steps if you are thinking about discontinuing your medication.
Why People Consider Stopping Antidepressants
Even if antidepressants have been effective, there are understandable reasons people want to stop:
Side effects such as weight gain, sexual difficulties, or fatigue.
Lifestyle preferences, such as wanting to “feel natural” or not rely on medication.
Belief that symptoms are resolved and treatment is no longer needed.
These are valid concerns, but the main issue psychiatrists worry about is relapse risk.
What the Evidence Says About Relapse
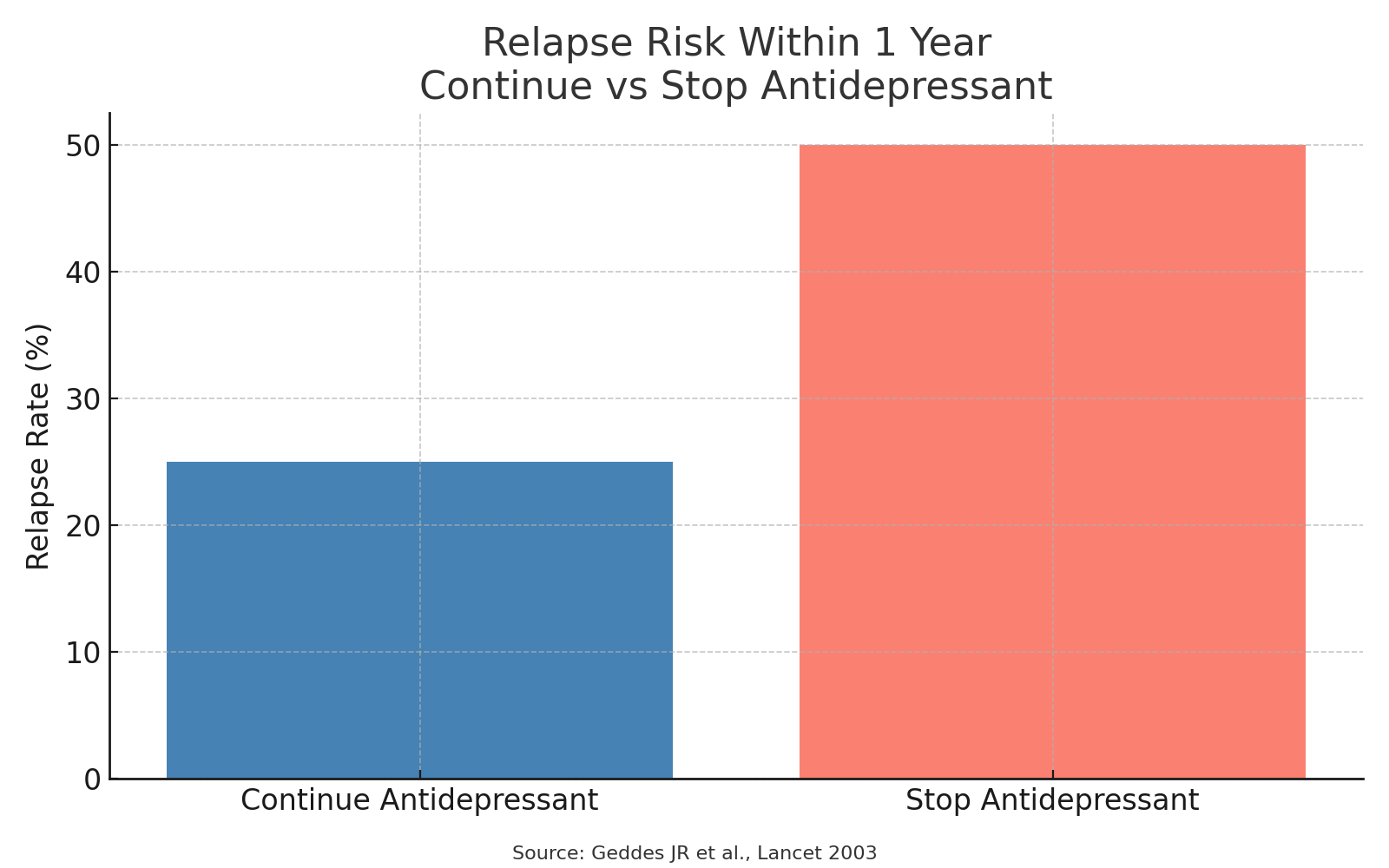
Research consistently shows that stopping antidepressants increases the likelihood of depression returning.
Meta-analyses (studies that combine results from multiple trials) find that people who discontinue antidepressants are about twice as likely to relapse compared with those who continue treatment.
The first 6 months after stopping is the period of highest risk.
People with multiple past depressive episodes, chronic depression, or co-occurring anxiety disorders are at especially high risk.
To give context: imagine 100 people who have recovered on antidepressants. If all continue their medication, about 20–30 may relapse within a year. If they stop, 40–60 may relapse within that same year.
Individual Risk Factors to Consider
Not every patient faces the same relapse risk. When I work with patients in my Manhattan office, we look closely at the following:
Number of previous depressive episodes
If you have had three or more, relapse risk is significantly higher.
Severity of past episodes
Hospitalization, suicidality, or inability to work or study are red flags.
Length of remission
Remaining well for over a year reduces risk, but it doesn’t eliminate it.
Comorbidities
Conditions like anxiety disorders, bipolar disorder, or substance use can complicate outcomes.
Psychosocial context
Living with high stress, discrimination, or lack of support can increase relapse risk. For example, many of my LGBT patients in NYC face unique stressors related to identity, family acceptance, or workplace environments.
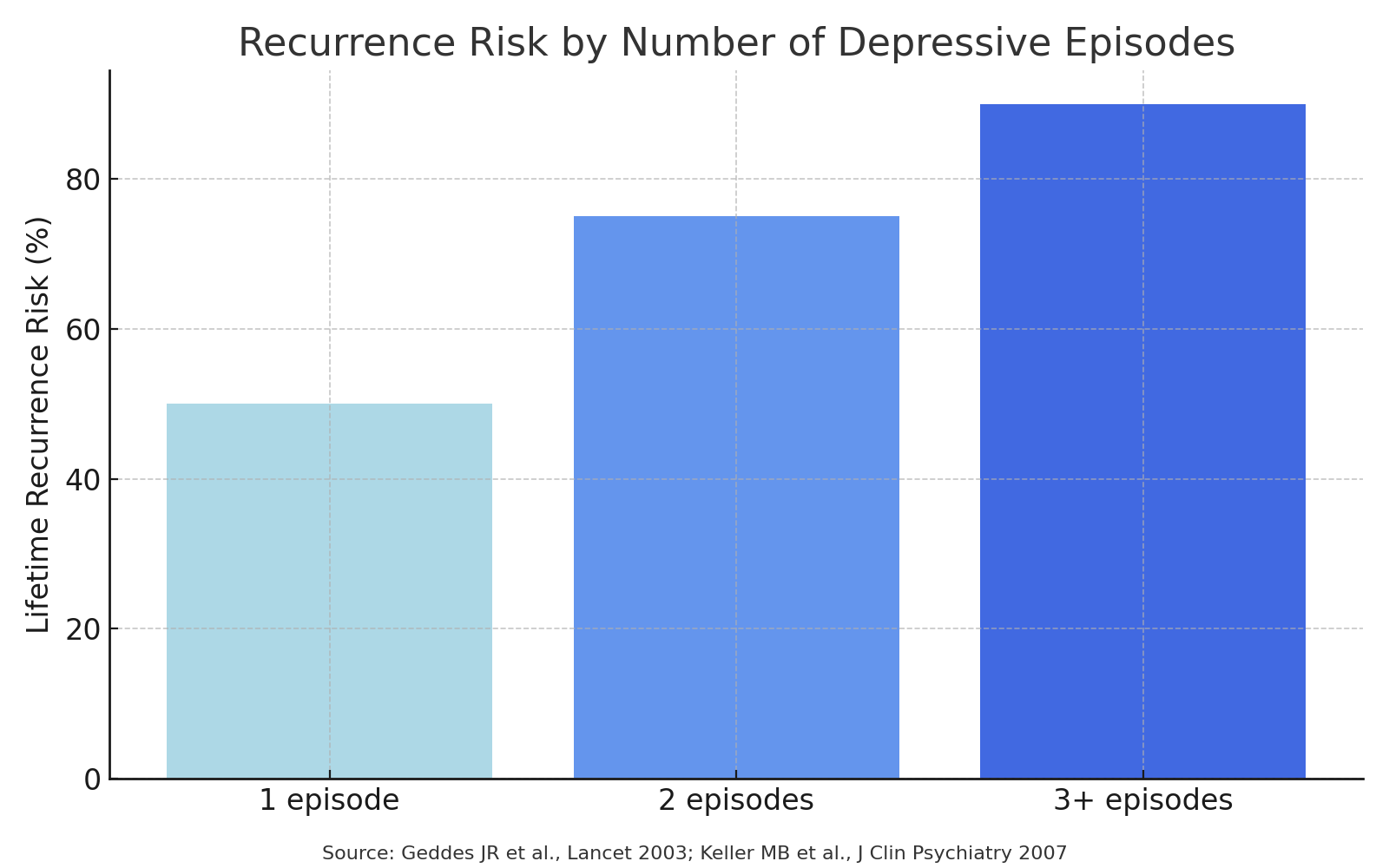
Number of Previous Episodes
Major risk factor: The strongest predictor of relapse is having multiple prior depressive episodes.
A landmark meta-analysis (Geddes et al., 2003, Lancet) found that:
After one episode, relapse risk is ~50%.
After two episodes, risk rises to ~70–80%.
After three or more episodes, risk is >90% across a lifetime.
In discontinuation studies, patients with ≥3 prior episodes relapse significantly faster and more frequently than those with one.
Severity of Past Episodes
More severe prior depression = higher relapse risk.
Indicators of severity include:
Hospitalization
Psychotic features
High suicidality
Marked functional impairment (e.g., inability to work, school dropout)
Keller et al. (2007, Journal of Clinical Psychiatry) and similar studies show that severity at baseline predicts both slower recovery and higher likelihood of recurrence.
Severe or melancholic depression tends to be more biologically recurrent, with higher relapse rates even if patients achieved remission on antidepressants.
Combined Effect
Multiple + severe past episodes compound relapse risk.
For example, someone with three severe episodes requiring hospitalization is much more likely to relapse off medication than someone with one mild episode treated in outpatient care.
Relapse risk within 1 year continue vs stop antidepressant
Clinical Guideline Implications
NICE (UK) and APA (US) guidelines recommend at least 2 years of maintenance treatment for patients with ≥2 episodes, and long-term or indefinite treatment for those with recurrent, severe, or chronic depression.
Patients with only one mild episode may try discontinuation after 6–12 months of remission, but close monitoring is essential.
So, in practice:
Number of episodes tells us about recurrence risk.
Severity of past episodes tells us about how disabling relapse might be.
Together, they’re the strongest predictors psychiatrists use when helping patients decide whether to continue or stop antidepressants.
Antidepressant Discontinuation Syndrome
Another reason to avoid abrupt stopping is withdrawal-like symptoms, known as antidepressant discontinuation syndrome.
These can include:
Dizziness or “brain zaps”
Flu-like feelings
Irritability or mood swings
Difficulty sleeping
Anxiety or agitation
They usually resolve in a couple of weeks but can be distressing and, importantly, may be confused with relapse. This is why psychiatrists stress gradual tapering.
Duration of Treatment: What Guidelines Recommend
Most psychiatric guidelines, including those from the American Psychiatric Association, advise:
First episode of depression: Continue antidepressants for at least 6–12 months after remission.
Recurrent depression: Consider 2 years or more of treatment.
Chronic or severe cases: Long-term or even indefinite treatment may be recommended.
This doesn’t mean you must be on medication forever, but it does highlight how quickly stopping after feeling better can backfire.
The Role of Psychotherapy and Lifestyle
Medication is one tool. If you’re considering discontinuing, your psychiatrist may recommend strengthening non-medication supports first:
Psychotherapy: Especially cognitive-behavioral therapy (CBT) or psychodynamic therapy. Therapy not only reduces relapse risk but also provides skills for long-term resilience.
Lifestyle changes: Regular exercise, consistent sleep, reduced alcohol, and mindfulness practices are protective.
Community support: For LGBT patients, affirming spaces in Manhattan and NYC—such as support groups or community centers—can buffer against stress.
Practical Steps if You Are Thinking About Stopping
Talk to your psychiatrist first
Don’t stop on your own. A Manhattan psychiatrist can help you evaluate risk and guide tapering.
Make a tapering plan
Reducing the dose slowly, over weeks to months, minimizes withdrawal.
Monitor symptoms closely
Keep a mood journal or use an app. Early warning signs of relapse include loss of interest, sleep changes, and fatigue.
Schedule follow-up visits
Regular check-ins ensure that if depression starts returning, adjustments can be made quickly.
Have a relapse prevention plan
Identify coping strategies, emergency contacts, and a plan for restarting treatment if needed.
Special Considerations for LGBT Patients in NYC
As a Manhattan LGBT psychiatrist, I often see how identity-related stress intersects with mental health. Coming off antidepressants may feel appealing when someone is thriving, but external pressures—such as discrimination or family rejection—can increase relapse risk.
Studies show that LGBT individuals have higher rates of depression and anxiety, often tied to minority stress. When weighing whether to stop medication, it’s important to factor in these social realities. Supportive psychotherapy and affirming care are especially valuable here.
Case Example
Consider Alex, a 28-year-old professional living in Manhattan. They identify as nonbinary and began antidepressants after a severe depressive episode two years ago that included suicidal thoughts. With a combination of escitalopram and weekly therapy, Alex’s mood stabilized.
Now, feeling stronger, Alex wonders: “Should I stop?”
We discussed:
Alex has had two major episodes, meaning relapse risk is higher.
Work stress and ongoing challenges around family acceptance are active risk factors.
Alex wants fewer side effects but values stability.
Together, we decided on a gradual dose reduction trial, paired with ongoing therapy, exercise goals, and frequent follow-ups. Six months later, Alex is still doing well, though we agreed to remain vigilant.
This illustrates that stopping antidepressants isn’t simply yes or no—it’s a nuanced process tailored to each individual.
My Approach as a Manhattan Psychiatrist
When patients ask if they should come off antidepressants, my role is not to push one direction but to provide evidence-based guidance. I emphasize:
Shared decision-making: You are the expert in your life; I bring the data.
Risk management: Understanding your relapse risk helps you make an informed choice.
Affirming care: Particularly for LGBT patients, ensuring a safe and supportive space to weigh these decisions is essential.
Key Takeaways
Stopping antidepressants increases relapse risk, especially within the first 6 months.
Multiple past episodes, severity, and ongoing stress raise risk further.
If you do discontinue, taper gradually with medical guidance.
Psychotherapy, healthy routines, and community support can reduce relapse risk.
For LGBT patients in NYC, affirming care and strong support networks are particularly protective.
Final Thoughts
If you’re asking, “Should I get off my antidepressants?”—you’re not alone. It’s a question that deserves careful attention, not quick answers. Evidence shows the risk of relapse is real, but with planning, support, and collaboration with a trusted NYC psychiatrist, many people can reduce or discontinue medication safely.
Whether you are early in your recovery or years into stability, it’s worth having an open conversation with a clinician who understands both the science and your personal context.
If you’re in New York and seeking guidance, consider reaching out to a Manhattan psychiatrist who can provide thoughtful, individualized, and affirming care.